TMS vs Spravato Explained: Key Differences Every Patient Should Know
Comparing TMS vs Spravato for depression? Learn how they differ in approach, effectiveness, side effects, and who each treatment may help.

If you are comparing TMS and Spravato, it usually means depression has not improved with standard treatment. These options tend to come up after medications or therapy have not brought enough relief, and the decision can feel more serious than simply trying another prescription.
This article takes a clear, practical look at TMS vs Spravato. It explains how each treatment works, what the experience is like, and which factors tend to matter most when choosing between them. The goal is not to persuade you toward a specific option, but to help you understand the differences well enough to have a more informed conversation with your provider.
The team at Charak Center for Health and Wellness offers individualized evaluations and evidence-based guidance for people exploring advanced depression treatments. You can learn more about their approach to mental health care at charakcenter.com.

Transcranial Magnetic Stimulation Overview
Transcranial Magnetic Stimulation, commonly referred to as TMS, is a non invasive treatment used to address major depressive disorder and certain other mood related conditions, particularly when standard treatments have not provided enough relief. TMS is FDA approved for depression and does not involve medication, sedation, or anesthesia. Treatment typically consists of a series of sessions, with response varying based on symptom severity, diagnosis, and treatment history.
Spravato Overview
Spravato is a prescription nasal spray containing esketamine, a medication used to treat major depressive disorder in adults, particularly when symptoms have not improved with standard antidepressant treatments.
It is FDA approved for treatment resistant depression and for depressive symptoms in adults with major depressive disorder accompanied by acute suicidal thoughts or behaviors. Spravato is administered in a clinical setting and is used alongside an oral antidepressant as part of a supervised treatment plan.
How Each Treatment Affects Brain Activity
Transcranial Magnetic Stimulation (TMS)
TMS works by delivering focused magnetic pulses to specific areas of the brain involved in mood regulation, most often the dorsolateral prefrontal cortex. A magnetic coil placed on the scalp generates electromagnetic pulses that influence nerve cell activity and communication within targeted brain circuits. With repeated stimulation over time, TMS is believed to help shift patterns of brain activity that are commonly associated with depressive symptoms.
Spravato
Spravato affects brain activity by acting on the glutamate system rather than the serotonin pathways targeted by most antidepressants. Its active ingredient, esketamine, interacts with NMDA receptors, which alters how nerve cells communicate in brain regions involved in mood and emotional regulation.
These changes are thought to support synaptic plasticity, helping the brain form new connections. This mechanism may explain why some people experience symptom improvement more quickly than with traditional medications.
What Going Through Treatment Is Actually Like
TMS follows a structured outpatient process designed to integrate into daily routines. Sessions are scheduled in advance and delivered as part of an ongoing treatment plan rather than a one time intervention. While protocols may vary, the overall treatment experience is consistent and predictable.

TMS
- Initial Evaluation: Treatment begins with a clinical evaluation that reviews diagnosis, symptoms, medical history, and prior treatments to determine whether transcranial magnetic stimulation is an appropriate option.
- Treatment Setup: During each visit, patients sit comfortably while the care team positions the TMS device and adjusts settings based on response, comfort, and treatment goals.
- Administration: A magnetic coil is placed against the head to deliver controlled pulses to targeted brain regions involved in mood regulation, following a defined protocol under clinical supervision.
- During the Session: Patients remain awake during quiet, structured sessions and can usually return to normal activities immediately. Mild scalp discomfort or headaches may occur early in treatment.
- Ongoing Sessions: TMS is typically delivered five days a week over several weeks, with progress monitored and settings adjusted as needed. Some individuals may benefit from maintenance sessions to support ongoing symptom improvement.
Spravato
- Initial Evaluation: Treatment begins with a clinical evaluation that reviews diagnosis, symptoms, medical history, and prior treatments to determine whether Spravato is appropriate.
- Treatment Session: During each visit, patients self administer the nasal spray under clinical supervision while seated comfortably in a medical setting.
- Monitoring Period: After dosing, patients remain on site for observation due to temporary effects on perception and blood pressure. Monitoring is a required part of treatment.
- After the Session: Most patients do not drive or return to work the same day and arrange transportation home. Short term effects usually resolve within a few hours.
- Ongoing Sessions: Treatment follows a structured schedule, with frequency adjusted over time based on response and tolerability.
Who May Benefit Most From Each Option
Choosing between TMS and Spravato is less about which treatment is better overall and more about how each option aligns with individual symptoms, treatment history, and practical considerations. Factors such as response to past treatments, tolerance for medication effects, and daily scheduling needs often play an important role in determining the best fit.
TMS may be a good option for individuals who:
- Have major depressive disorder, including treatment resistant depression
- Have not experienced enough improvement after trying multiple antidepressants
- Have difficulty tolerating medication side effects or prefer a non medication approach
- Are looking for a structured, non invasive treatment option
Spravato may be a good option for individuals who:
- Have major depressive disorder that has not improved with standard antidepressant treatment
- Need faster symptom relief as part of a closely monitored treatment plan
- Can tolerate short term medication effects and clinical observation after each dose
- Are able to attend supervised in clinic sessions and arrange transportation home
Ultimately, the right choice depends on individual needs, treatment history, and how each option fits into daily life.
Side Effects and Safety Considerations
Both TMS and Spravato are generally well tolerated, but they come with different side effect profiles based on how each treatment works. Understanding these differences can help set realistic expectations before starting care.
Common Side Effects of TMS
Side effects associated with TMS are typically mild and localized to the treatment area.
- Scalp discomfort: Mild tenderness or pressure where the magnetic coil is placed, often described as mild discomfort during or shortly after a tms session
- Headaches: Usually mild headache symptoms that tend to occur early in tms treatment and often improve as sessions continue
- Facial muscle twitching: Brief muscle activation during stimulation, limited to the session itself
These effects often lessen over time as treatment progresses. Since TMS is not medication derived, it does not cause systemic side effects such as weight gain, sedation, or gastrointestinal issues that are sometimes associated with traditional antidepressant medications
Common Side Effects of Spravato
Spravato side effects are related to its effects on the central nervous system and blood pressure. These effects are usually short term and monitored during treatment sessions.
- Dissociation or altered perception: Temporary changes in awareness or sensory experience that may occur shortly after dosing
- Dizziness or nausea: Sensations of lightheadedness or nausea, most common early in the session
- Increased blood pressure: Short term elevations that are monitored before and after each dose, particularly important for individuals with high blood pressure
- Fatigue or sedation: Temporary tiredness that can affect recovery time and same day activities
Due to these effects, Spravato is administered under supervision with a required observation period after each dose. This allows healthcare providers to monitor safety while supporting many patients with severe depression, depression symptoms, or acute suicidal ideation who have not seen sufficient improvement with traditional antidepressants, antidepressant medications, or talk therapy.
Side effects vary from person to person, and not everyone experiences them. A clinical provider can help weigh potential benefits against risks based on medical history, symptom severity, and prior treatment response.
TMS vs Spravato: Practical Differences to Consider
In 2024, an estimated 23.4% of U.S. adults experienced mental illness, representing more than 61 million people. As more individuals seek care, it has become increasingly clear that even limited personal data can reveal sensitive information about someone’s life and health. Side effects can influence not only comfort during treatment but also how manageable each option feels over time. The table below highlights differences that tend to matter most in day to day decision making.
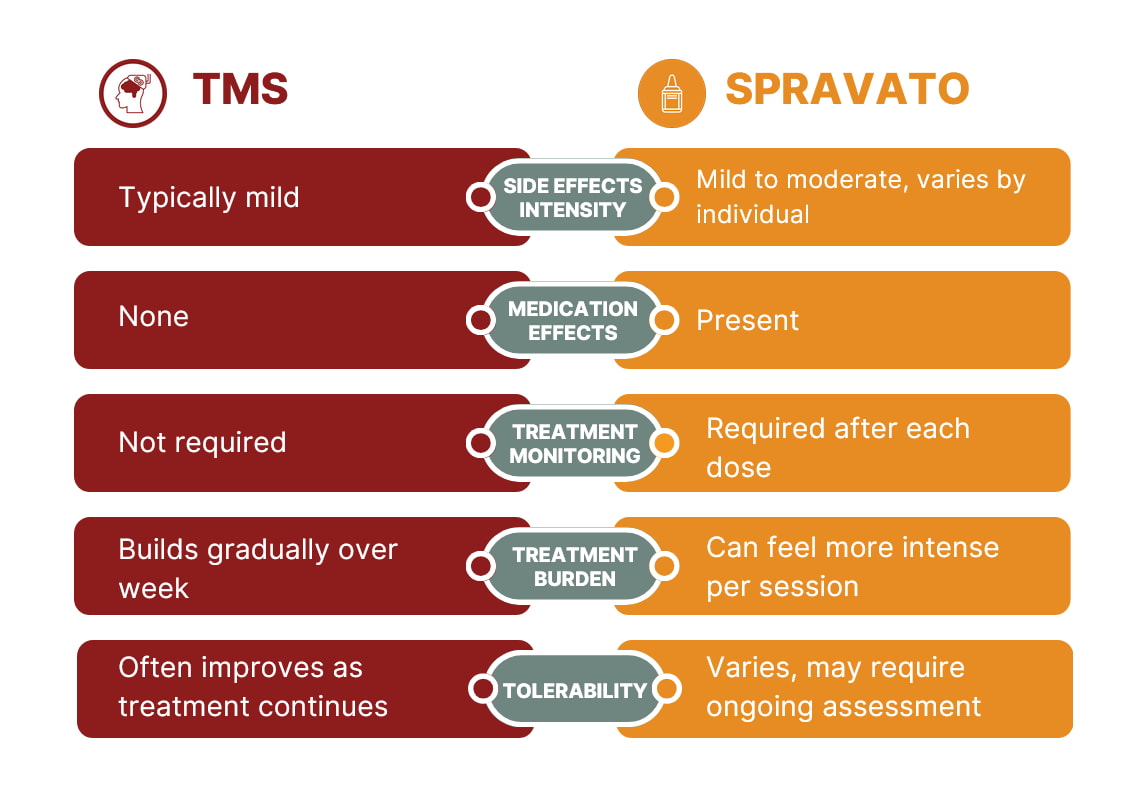
While both treatments are considered safe when appropriately prescribed, the overall experience and level of monitoring can differ in ways that may affect which option feels more sustainable for an individual.
Which Treatment Makes Sense for You
Choosing between TMS and Spravato is not about finding a single right answer. Each option works differently and places different demands on daily life, which means the better fit often depends on personal factors rather than symptom severity alone.
Some people prioritize a non medication approach that allows them to maintain a consistent routine, while others may be focused on faster symptom relief under close medical supervision. Treatment history, response to past medications, tolerance for monitoring, and scheduling needs all play a role in this decision. For individuals managing complex mental health needs, additional support such as coordinated case management services can help address practical barriers, align care across providers, and support continuity throughout treatment.
A thorough clinical evaluation can help clarify which option aligns best with your symptoms, preferences, and long term treatment goals. If you would like to speak with a provider, you can call 1-855-4CHARAK (1.855.424.2725) or fill out the contact form to request more information.





