TMS vs Other Treatments: A Clear, Evidence-Based Breakdown
TMS vs other treatments explained in simple, evidence-based terms. Find out how TMS may offer stronger results for anxiety and depression.

When anxiety or depression starts interfering with daily life, choosing a treatment can feel like trying every door in the dark and hoping one finally leads somewhere better. Many people begin looking for an option that does more than manage symptoms for the moment. That search is what brings so much attention to Transcranial Magnetic Stimulation, or TMS. It takes a different approach by directly influencing the brain circuits involved in mood and emotional regulation.
This guide breaks it down clearly so you can understand the real differences, the limitations, and the situations where TMS might offer a level of relief that other treatments do not.
If you are weighing TMS against other treatment options and want support choosing a path that fits your symptoms and goals, a clinician can help you sort through the differences. You can learn more about our approach to anxiety care at charakcenter.com.

What TMS Is (and What It Isn’t)
What TMS Is
Transcranial Magnetic Stimulation (TMS) is a noninvasive brain-stimulation treatment that uses targeted magnetic pulses to influence areas of the brain involved in mood and emotional regulation, most often the dorsolateral prefrontal cortex.
TMS is FDA-cleared for major depressive disorder, including treatment-resistant depression. Clinical studies show that response rates vary, with roughly 30 to 60 percent of patients experiencing meaningful improvement. Because depression and anxiety can involve overlapping brain circuits, some clinicians also use TMS to address anxiety symptoms, although research in this area is still evolving.
What TMS Isn’t
TMS is not medication and not a quick fix. Results, when they occur, develop gradually over several weeks. It’s also not a guaranteed cure and works differently for each person. TMS is best viewed as one treatment option that may be used alongside other therapies.
How TMS Compares to Other Mental Health Treatments
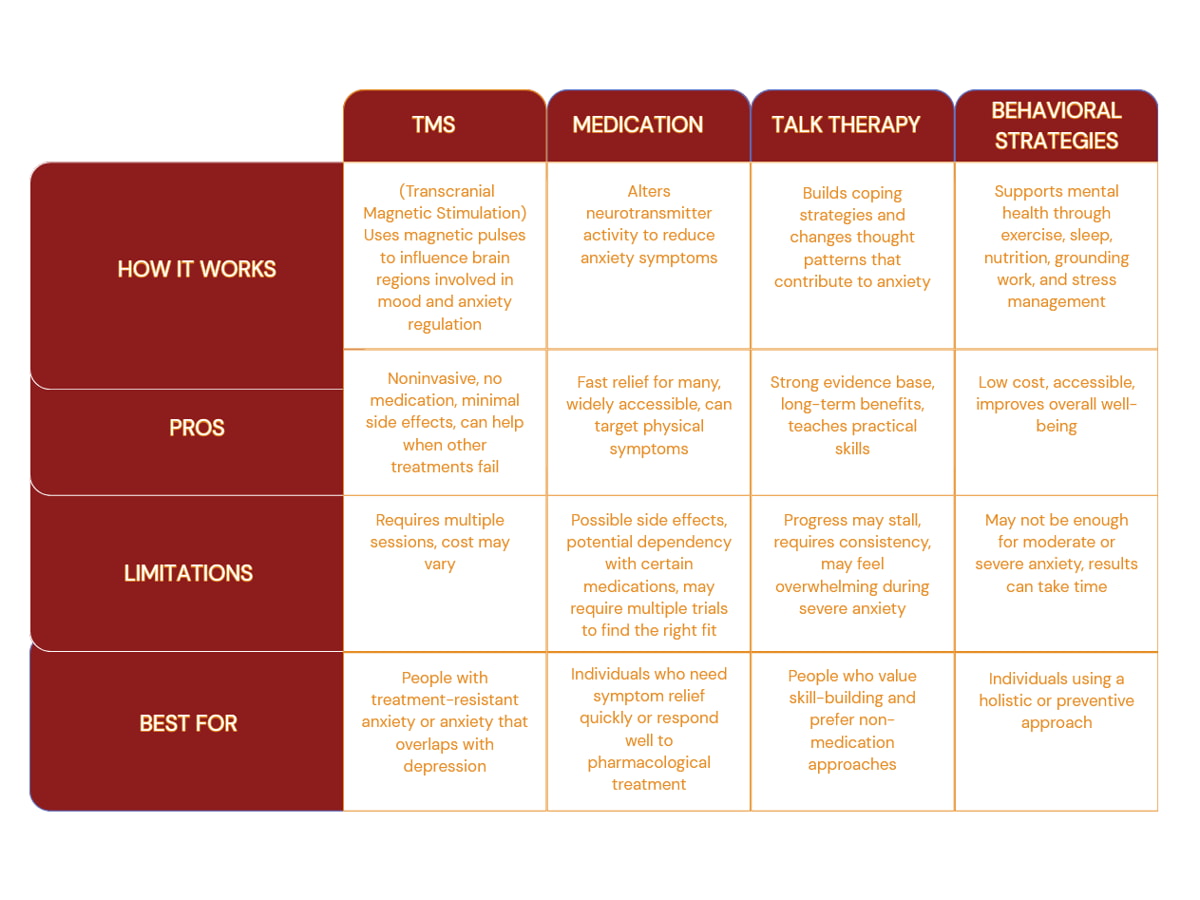
There’s no single “right” treatment for anxiety or depression. What matters is how each option works and what it’s designed to address.

TMS vs. Medication
Clinical studies report remission rates of around 42.8 percent following rTMS therapy, though outcomes vary by individual and treatment history. Medication changes brain chemistry throughout the body, which can reduce symptoms but may also lead to side effects such as sexual dysfunction, weight changes, or fatigue. TMS works differently by using targeted magnetic pulses to stimulate specific brain areas involved in mood regulation. Because the treatment is localized, it tends to avoid many of the systemic effects associated with antidepressants. Medication is often a first-line option, while TMS is typically considered when medications are not effective or are poorly tolerated.
TMS vs. Talk Therapy
Research suggests that roughly three out of four people benefit from psychotherapy in some form. Talk therapy helps people understand patterns, build coping skills, and change behavior. TMS works differently by targeting brain activity that can make those changes harder to access when symptoms are severe or persistent. When therapy alone does not lead to enough progress, TMS may help reduce symptom intensity so therapy becomes more effective rather than feeling overwhelming.
TMS vs. Behavioral and Lifestyle Strategies
Sleep, exercise, nutrition, and stress management all play an important role in mental health. For many people, these strategies help support long-term stability. But when symptoms are moderate to severe, lifestyle changes alone may not be enough. TMS addresses underlying brain activity and is usually considered when healthy habits don’t provide meaningful relief on their own.
How TMS Treatment Is Structured
A typical TMS treatment plan is structured, predictable, and designed to fit into daily life.

1. Initial Evaluation
Treatment starts with a clinical assessment to confirm whether TMS is appropriate based on diagnosis, symptom history, and prior treatments. If approved, the provider identifies the target brain area and determines the right stimulation settings.
2. Treatment Schedule
Most plans involve daily sessions, five days a week, over several weeks. Each session usually lasts 20 to 40 minutes. You remain awake the entire time and can return to normal activities immediately afterward.
3. During Sessions
You’ll sit comfortably while a magnetic coil delivers brief pulses to a specific area of the scalp. Many people describe the sensation as a tapping or clicking feeling. Discomfort is usually mild and often decreases after the first few sessions.
4. Monitoring Progress
Improvement isn’t immediate. Some people notice changes within the first few weeks, while others experience gradual improvement closer to the end of treatment. Results vary, and symptom relief tends to build over time rather than happen all at once.
5. After Treatment
Some individuals experience sustained improvement, while others may benefit from maintenance sessions in the future. Your provider will monitor progress and adjust recommendations as needed.
Overall, TMS treatment follows a clear, step-by-step process that allows providers to adjust care based on how symptoms respond over time, helping ensure treatment stays both effective and manageable. For patients who need additional coordination or ongoing support alongside treatment,case management services can help address practical needs, continuity of care, and long-term planning.
Could TMS Be the Next Step in Your Treatment?
If medication, therapy, or lifestyle changes have not provided enough relief, TMS may be worth considering. It is often explored when symptoms persist, medication side effects limit treatment options, or progress has stalled despite consistent care. TMS does not replace what you have already tried. It can complement existing treatment by targeting brain activity linked to ongoing symptoms.
Questions about whether TMS could help? Call 1-855-4CHARAK (1-855-424-2725) or fill out the contact form to get clear, personalized guidance from our care team.
Your Questions About TMS, Answered
Q1: Does TMS hurt?
A: TMS therapy is a non invasive treatment and is generally well tolerated. During TMS sessions, an electromagnetic coil is placed near the patient’s head to deliver magnetic pulses that stimulate nerve cells involved in mood regulation. Most patients describe the sensation as tapping or clicking on the scalp. Discomfort is usually mild and often fades after the first few treatment sessions. Mild headaches can occur early on.
Q2: How long does it take to see results from TMS?
A: Response varies depending on the individual, their medical history, and the condition being treated. Some patients notice changes in depression symptoms within a few weeks, while others experience improvement closer to the end of multiple sessions. TMS is designed to work gradually, and many patients report significant improvements over time rather than immediate relief.
Q3: Can I continue medication or therapy during TMS?
A: Yes. TMS is often used alongside conventional treatments, including talk therapy and multiple medications. It is commonly considered for treating major depressive disorder when standard depression treatment options have not been effective. Your healthcare provider will review your medical history and coordinate care as part of a personalized treatment plan.
Q4: Are there side effects with TMS?
A: Side effects from TMS therapy are usually mild and temporary. The most common effects include scalp discomfort or mild headaches during early treatment sessions. TMS does not typically cause memory loss, weight gain, sexual dysfunction, or sedation, and it does not require general anesthesia. Serious side effects are rare when treatment is provided by trained TMS providers.
Q5: Is TMS a long term solution?
A: Many patients experience long term benefits after completing a full course of treatment sessions. If symptoms return, follow up or maintenance sessions may be recommended. Long term outcomes and response rates vary, but many patients report positive results and improved quality of life.





