Ketamine vs TMS: Understanding Your Mental Health Treatment Options.
Ketamine vs TMS explained. Compare benefits, risks, side effects, and how each treatment fits depression and anxiety care.

When standard treatments stop working, the conversation shifts quickly to options most people were never told about. Ketamine and TMS are often presented as the next step, yet they are fundamentally different treatments with very different goals, timelines, and risk profiles.
This article breaks down ketamine vs TMS with a clinical lens and plain language, so you can understand what separates these treatments, what the research supports, and how clinicians think about choosing between them when conventional approaches have not been enough.
Charak Center for Health and Wellness takes a personalized approach to mood and anxiety care, focusing on evidence-based treatment planning rather than one-size-fits-all solutions. You can learn more about our approach at charakcenter.com.
Ketamine Therapy Explained
Ketamine therapy is a medical treatment used to help manage severe or treatment-resistant depression and certain mood disorders. At low doses, ketamine is administered under medical supervision, most commonly through intravenous infusion or as FDA-approved esketamine nasal spray. Treatment plans typically involve multiple sessions, with responses varying based on symptoms and medical history.
How Ketamine Affects Brain Chemistry
Ketamine works primarily on the brain’s glutamate system rather than serotonin. It blocks NMDA receptors, which changes how nerve cells communicate and promotes increased signaling in pathways linked to mood regulation. This process is thought to support improved neural connectivity and may help explain why ketamine can produce antidepressant effects more quickly than many conventional treatments.
Ketamine Treatment Experience
Ketamine treatment follows a structured, medically supervised process designed to fit within an outpatient setting. Sessions are planned in advance and delivered as part of a broader treatment plan rather than as a one-time intervention. While individual protocols vary, the overall experience is generally consistent.
1. Initial Evaluation
Treatment begins with a clinical evaluation that reviews symptoms, diagnosis, and medical history. This assessment helps determine whether ketamine is appropriate, including consideration of conditions such as bipolar disorder, history of substance abuse, or active suicidal ideation. Prior response to other treatments, including electroconvulsive therapy (ECT) or electroconvulsive therapy ect, may also be reviewed.
2. Treatment Setup
On treatment days, patients are checked in and seated or reclined in a quiet medical environment. The care team prepares the session based on the prescribed plan, including route of delivery and ketamine dose, while reviewing potential drug interactions and treatment goals.
3. Administration
Ketamine is most commonly delivered through intravenous ketamine as part of ketamine infusions, though some protocols involve alternative forms of ketamine administration. Sessions follow a defined timeline and are supervised by trained medical staff. Some patients may respond after a single ketamine infusion, while others require a series of treatments depending on response and treatment duration.
4. During the Session
Patients remain seated or reclined throughout the session. The setting is typically calm and low-stimulus, allowing patients to rest while treatment is administered. Ketamine’s effects on glutamate pathways and brain derived neurotrophic factor are an area of active research and may help explain its role in reducing depressive symptoms.
5. Ongoing Sessions
Most treatment plans involve multiple sessions over several weeks. Progress is reviewed regularly, and the plan may be adjusted based on response, side effects, and overall treatment outcomes. In some cases, ketamine may be explored as part of combination therapy or combined treatment alongside other approaches such as transcranial magnetic stimulation TMS, including rTMS treatment or intermittent theta burst stimulation, as supported by emerging clinical trials and randomized controlled trial data.
Who Ketamine Therapy Is Best Suited For
Ketamine therapy is most often considered when standard treatments have not provided enough relief. It is typically used after other approaches have been tried rather than as an initial option.
Ketamine may be appropriate for individuals who:
- Have treatment-resistant depression, with limited response to multiple medications or therapy
- Experience severe or persistent depression symptoms that significantly affect daily functioning
- Have not tolerated conventional antidepressants or have seen diminishing benefits over time
- Need an alternative approach when traditional treatments have stalled
Depression is a widespread condition, affecting an estimated 280 million people worldwide, and many do not find adequate relief with standard treatments. Because ketamine works through a different neurochemical pathway than most antidepressants, it may be considered when conventional options have not been effective. A clinical evaluation helps determine whether ketamine aligns with a person’s diagnosis, medical history, and treatment goals.
Common Side Effects of Ketamine Treatment
Ketamine treatment can cause side effects, though not everyone experiences them. When they do occur, they are typically short term and monitored during treatment sessions.
- Perceptual changes: Temporary changes in awareness or sensory perception during a session
- Dizziness or lightheadedness: Brief feelings of imbalance that usually resolve shortly after treatment
- Nausea: Mild stomach discomfort that may occur during or shortly after a session
- Blood pressure changes: Short-term increases in blood pressure or heart rate during treatment
Most side effects fade soon after a session ends. A healthcare provider reviews medical history and monitors treatment closely to support safety and comfort throughout the process.

TMS Therapy Explained
Transcranial Magnetic Stimulation, or TMS, is a non invasive treatment used to help manage major depressive disorder and other mood disorders, particularly when standard treatments have not been effective. TMS is FDA approved for treating depression and does not require medication, sedation, or anesthesia. Treatment plans typically involve multiple sessions, with outcomes varying based on symptoms and treatment history.
How TMS Affects Brain Activity
TMS works by using focused magnetic fields to stimulate nerve cells in specific brain regions involved in mood regulation, most commonly the dorsolateral prefrontal cortex. An electromagnetic coil placed against the scalp delivers magnetic pulses that influence neural activity and communication between nerve cells. Over time, repetitive stimulation is thought to help normalize patterns of brain activity associated with depression symptoms.
TMS Treatment Experience
TMS treatment follows a structured, outpatient process and is designed to fit into daily life. Sessions are scheduled in advance and delivered as part of a consistent treatment plan rather than a single intervention. While protocols can vary, the overall experience is predictable.
1. Initial Evaluation
Treatment begins with a comprehensive clinical assessment that reviews diagnosis, depressive symptoms, medical history, and prior treatments. This evaluation helps determine whether TMS transcranial magnetic stimulation is appropriate for individuals with major depression, chronic depression, or other mental health disorders.
2. Treatment Setup
On treatment days, patients sit comfortably in a treatment chair. The care team positions the TMS device and calibrates individualized settings based on the patient’s response and treatment goals as part of a typical TMS treatment plan.
3. Administration
An electromagnetic magnetic coil is placed against the patient’s head to deliver focused pulses to targeted brain regions involved in mood regulation. This form of brain stimulation, often referred to as repetitive transcranial magnetic stimulation (rTMS), follows a defined schedule and is supervised by trained clinical staff.
4. During the Session
Patients remain awake and seated throughout TMS sessions. Visits are typically quiet and structured, and most patients are able to resume normal activities immediately afterward. Some individuals may experience a mild headache, particularly early in treatment.
5. Ongoing Sessions
A typical TMS treatment course involves sessions five days a week over several weeks. Treatment outcomes are monitored regularly, and adjustments may be made based on response. Some patients may benefit from maintenance sessions to support longer-term improvement in depression symptoms.
Who TMS Therapy Is Best Suited For
TMS is most often considered for individuals who have not experienced sufficient improvement with conventional treatments. It is typically explored after medication and therapy have been tried.
TMS may be appropriate for individuals who:
- Have major depressive disorder, including treatment-resistant depression
- Have tried multiple medications without adequate relief
- Cannot tolerate antidepressant side effects or prefer a non medication option
- Need a structured, non invasive treatment approach
Major depression affects a large portion of the U.S. population, making careful treatment selection especially important. A clinical evaluation helps determine whether TMS aligns with a person’s diagnosis, medical history, and treatment goals.
Common Side Effects of TMS Treatment
TMS treatment is generally well tolerated. Side effects, when they occur, are usually mild and temporary.
- Scalp discomfort: Mild tenderness or sensitivity at the treatment site
- Headaches: Usually mild and more common early in treatment
- Facial muscle twitching: Brief muscle activation during stimulation
Most side effects lessen as treatment continues. A healthcare provider monitors progress throughout the course of care to help ensure comfort and safety.
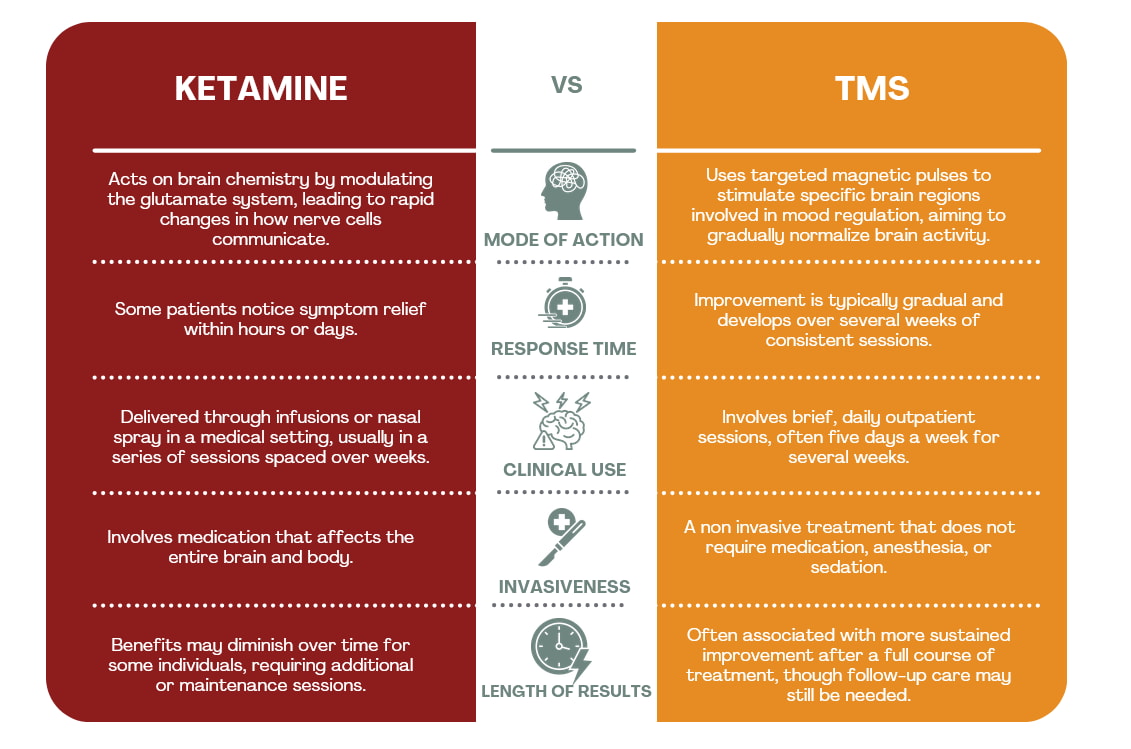
Ketamine vs TMS: How These Treatments Compare
While both treatments are used when standard approaches fall short, they differ in how they work, how quickly results appear, and how long benefits tend to last.
When Each Is Typically Considered
- Ketamine: Often explored when rapid symptom reduction is needed or when multiple medications have failed.
- TMS: Commonly considered for treatment-resistant depression when patients want a non medication option or have not tolerated antidepressants.
Finding the Right Fit for Your Treatment Goals
Choosing between ketamine and TMS is less about which treatment is better and more about which approach fits your symptoms, treatment history, and goals. Ketamine may be considered when faster symptom relief is a priority, while TMS is often chosen for its structured, noninvasive design and potential for longer-lasting results. For individuals with a history of substance use or concerns about medication safety, coordinated care that includes specialized substance use treatment may also be an important part of the decision-making process.
If you are considering ketamine, TMS, or other advanced treatment options and want guidance tailored to your symptoms and treatment history, a consultation can help clarify your next steps. To speak with a care team member, call 1-855-4CHARAK (1.855.424.2725 or fill out the contact form to request an evaluation.





